24 Dec Health: Building a Healthier Nation.
This article covers “Daily Current Affairs,” and the topic details related to, Health: Building a Healthier Nation.
Syllabus mapping:
GS-2: governance: Government policies and schemes related to the health sector.
For Prelims:
What articles of the Constitution of India dealt with the health sector, the seventh schedule, and subjects mentioned related to health?
For Mains:
What initiatives has the government of India taken to promote the health sector, its challenges, and measures to address these challenges?
Why in the News:
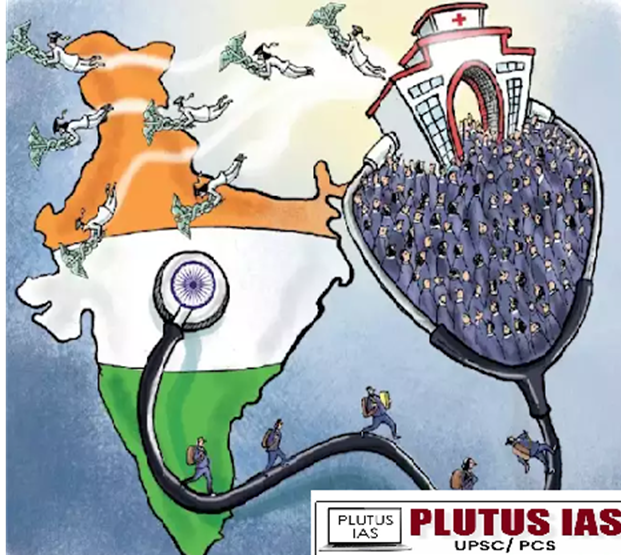
India’s progress in building a healthier nation has gained attention due to significant advancements in healthcare access, equity, and outcomes. Over the past decade, the country has introduced transformative policies reflecting a strong commitment to Universal Health Coverage. A major highlight in this journey is the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY), a flagship initiative that continues to play a pivotal role in reshaping India’s healthcare landscape.
Constitutional provisions related to the Health:
| Provisions | Description | Context for Health |
|---|---|---|
| Article 38 | The state is responsible for creating a social order that promotes the welfare of the people. | Framework for health and welfare-related policies, ensuring the welfare of people, including health, is prioritized. |
| Article 39(e) | The state is responsible for protecting the health and strength of workers, ensuring children’s health. | Ensures workers’ health and children’s well-being by providing adequate resources for healthy development. |
| Article 41 | The state is responsible for providing public assistance to the sick, disabled, and elderly. | Focuses on providing a safety net for the sick, disabled, and elderly, promoting social security for vulnerable populations. |
| Article 42 | The state is responsible for providing maternity benefits and ensuring humane working conditions. | Aims to improve women’s health, particularly during maternity, and ensure just working conditions. |
| Article 47 | The state is responsible for improving public health, raising standards of living, and regulating harmful substances. | Directly mandates the government to focus on public health, nutrition, and prohibit harmful substances like drugs. |
| Article 48A | The state is responsible for ensuring a pollution-free environment for good health. | Links environmental protection with public health, ensuring a healthy environment for citizens. |
| Union List (List I) | Central government’s role in regulating national health services, medical education, health research, pharmaceuticals, and managing health emergencies. | Union government has authority over national-level health services and emergency health management. |
| State List (List II) | State government’s role in managing public health services, including vaccination, maternal health, and disease control within their jurisdiction. | States are responsible for managing local healthcare services, including disease control and maternal health. |
| Concurrent List (List III) | Shared responsibility between the Union and State governments for regulating public health issues, such as narcotics control, disease prevention, and health insurance. | Both Union and State governments collaborate on health issues like disease prevention and public health regulation. |
Key Achievements of the Government in Healthcare
| Area | Achievement | Data/Details |
|---|---|---|
| Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) | – Health coverage of ₹5 lakh per family for secondary and tertiary care across 1,961 procedures in 27 specialties. | – 36.28 crore Ayushman Cards issued. – Women account for 49% of cards and 50% of admissions. – 30,932 hospitals empaneled. |
| Digital Health Infrastructure (ABHA) | – Facilitates access and sharing of digital health records. – Bridges gaps in the healthcare ecosystem through digital highways. |
– 71.81 crore ABHA numbers generated. – 46.53 crore health records linked. – 3.55 lakh health facilities and 5.38 lakh healthcare professionals registered. – PMNDP Portal, launched on 5th May 2022, integrates dialysis centers under NHM with ABHA ID for portability. |
| National Health Mission (NHM) | – Strengthens healthcare at district and community levels. | – 753 NCD clinics at district level and 6,238 NCD clinics at CHC level. – 220 Cardiac Care Units (CCUs) and 356 Day Care Cancer Centres established. |
| Mission Indradhanush | – Expanded immunization for children and pregnant women in low-coverage areas. – Provides protection against 11 preventable diseases. |
– Vaccinated 5.46 crore children and 1.32 crore pregnant women in all phases. |
| Improvement in Health Indicators | – Reduction in mortality rates and fertility rates due to targeted interventions. | – MMR reduced from 103 (2017-2019) to 97 (2018-2020). – IMR reduced from 32 (2018) to 28 (2020). – TFR reduced from 2.2 (2015-2016) to 2.0 (2019-2021). |
| National Family Health Survey (NFHS-6) | – Conducts large-scale surveys to monitor health indicators across districts. | – Pre-test conducted in June-July 2022; main survey fieldwork in progress. – Covers 731 districts with 6.77 lakh households. – Fieldwork completed in 20 States/UTs, ongoing in 15 others. |
| Tobacco-Free Youth Campaign | – Created awareness on the harmful effects of tobacco, focusing on youth and rural areas. | – Launched on 31st May 2023 (World No Tobacco Day). – 60-day campaign conducted across all States/UTs from May-July 2023. |
| Consumer-Centric Policies | – Data-driven and regularly monitored policies ensure inclusivity and sustainability. | – Commitment to achieving Universal Health Coverage through evidence-based strategies. |
Persistent Challenges in Healthcare
Doctor-to-Population Ratio: The World Health Organization (WHO) recommends a doctor-to-population ratio 1:1,000. India has a ratio of 1:1,511 (as of 2023), indicating a significant shortfall in healthcare providers, especially in rural areas.
Gender Gap in Access to Healthcare: Women account for only 49% of Ayushman Bharat Cardholders despite being 50% of the population, reflecting gender disparities in accessing healthcare services.
Urban-Rural Divide in Healthcare Services: 70% of India’s population resides in rural areas, but 60% of hospitals and healthcare infrastructure are concentrated in urban areas. Rural India faces a shortage of 83% of specialist doctors at Community Health Centers (CHCs), according to the Rural Health Statistics (2022).
Regional Divide (Northeast and Remote Areas): Northeastern and remote states have fewer medical colleges and specialized hospitals compared to central and southern states. For example, Arunachal Pradesh has only 1 medical college for a population of over 1.3 million.
Caste-Based Inequality in Healthcare Access: Marginalized communities, such as Dalits, report higher rates of exclusion from healthcare services. The National Family Health Survey-5 (NFHS-5) highlighted that only 28% of Dalit households have access to private health care compared to 50% of upper-caste households.
Slow Growth in Public Health Infrastructure: Public health expenditure in India remains low at 1.28% of GDP (2022-2023), far below the global average of 6%. India has only 1 government hospital bed per 1,844 people, compared to the global average of 1:550.
High Out-of-Pocket Expenditure (OOPE): OOPE accounts for 48.8% of total health expenditure in India, as per the National Health Accounts (NHA) 2022. This disproportionately affects low-income families, pushing an estimated 63 million people into poverty annually due to healthcare costs.
Lack of Health Insurance Coverage: Despite schemes like Ayushman Bharat, only 41.1% of Indian households have at least one member with health insurance, as per NFHS-5. Informal sector workers and rural populations often remain uninsured, leading to higher financial vulnerabilities.
Overemphasis on Secondary and Tertiary Care: A disproportionate focus on hospitals and high-end treatments often overshadows the need for robust primary healthcare systems. Only 3% of the health budget is allocated to preventive and promotive health services, while secondary and tertiary care dominates expenditures.
Privatization of Medical Education: The high cost of private medical education limits access for economically weaker sections. Over 60% of medical colleges in India are private, creating an uneven distribution of healthcare professionals and increasing healthcare costs.
Curative Treatment Over Preventive Services: India’s healthcare system primarily focuses on curative treatments rather than preventive care. For example, non-communicable diseases (NCDs) account for over 60% of deaths, yet there is limited emphasis on preventive strategies like lifestyle interventions and early screenings.
Way Forward
Universal Health Coverage (UHC): As envisioned in the National Health Policy, prioritize achieving UHC by ensuring equitable access to quality healthcare for all citizens, irrespective of socioeconomic or regional disparities.
Strengthening Primary Healthcare: Focus on primary healthcare as the backbone of the health system, particularly to address the needs of rural populations, which constitute over 60% of India’s population.
Gradual Improvement in Health Infrastructure: Invest in improving health infrastructure incrementally, including building medical colleges, increasing hospital capacities, and enhancing diagnostic and treatment facilities in underserved regions.
Promotion of Alternative Medicine Systems: Promote traditional systems of medicine like AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy) for a holistic approach to healthcare.
Enhanced Focus on Women and Children: Strengthen programs like ASHA (Accredited Social Health Activists) workers to ensure better access to healthcare for women and children in remote areas.
Emphasis on Preventive Care: Shift the focus from curative treatments to preventive and promotive healthcare to address the growing burden of non-communicable diseases (NCDs).
Inclusive Healthcare for Marginalized Groups: Adopt an inclusive approach as recommended by various committees, ensuring healthcare access for tribal communities, Dalits, and economically weaker sections.
Leverage Technology and Data: Utilize digital platforms like ABHA and telemedicine to bridge the urban-rural healthcare divide.
Increase Public Health Expenditure: Raise public health expenditure to at least 2.5% of GDP as recommended by the National Health Policy to strengthen the healthcare system sustainably.
Collaboration with the Private Sector: Build partnerships with private healthcare providers to expand access and reduce the burden on public healthcare infrastructure. Regulate and subsidize private healthcare services to ensure affordability and transparency.
Download Plutus IAS Current Affairs (ENG) 24rd Dec 2024
Conclusion:
In recent years, several initiatives have improved the status of the health sector in India. However, the need is to address the persistent challenges and make the health sector affordable, accessible, and inclusive to all people.
Prelims Question:
Q. Consider the following subjects:
1. Public health and sanitation
2. Hospitals and dispensaries
3. Medical Education
How many of the above subjects are mentioned in the Union List of the Seventh Schedule?
A. Only one
B. Only two
C. All three
D. None
ANSWER: D
Mains question:
Q.1. Assess the role of the National Medical Commission (NMC) Act of 2019 in promoting accessible and affordable health services in India.
(Answer in 250 words)



No Comments