23 May New Antibiotics vs. Evolving Resistance: A Race Against Time
This article covers “Daily Current Affairs” and the Topic New Antibiotics vs. Evolving Resistance: A Race Against Time.
SYLLABUS MAPPING:
GS-3- Science and technology-New Antibiotics vs. Evolving Resistance: A Race Against Time
FOR PRELIMS
What is Antimicrobial Resistance (AMR), and why is it a serious health concern in India?
FOR MAINS
What are the challenges faced in managing AMR in India?
Why in the News?
The death of 55-year-old Viswanatham from rural India has spotlighted the growing threat of Antimicrobial Resistance (AMR). After a respiratory illness in 2020, he sought help from a rural private practitioner, which led to complications and a leg infection. As a diabetic with a weak immune system, he was given a last-resort antibiotic that damaged his kidneys. Hospital-acquired infections further worsened his condition, and he died in 2021. His case underscores the dangers of irrational antibiotic use and the spread of resistant infections in both community and hospital settings. According to the Institute for Health Metrics and Evaluation (IHME), AMR caused 4.1 million deaths directly and 2.8 million associated deaths in 2019. The crisis has gained renewed attention, calling for urgent measures in antibiotic regulation, infection control, and public awareness.

What is AMR?
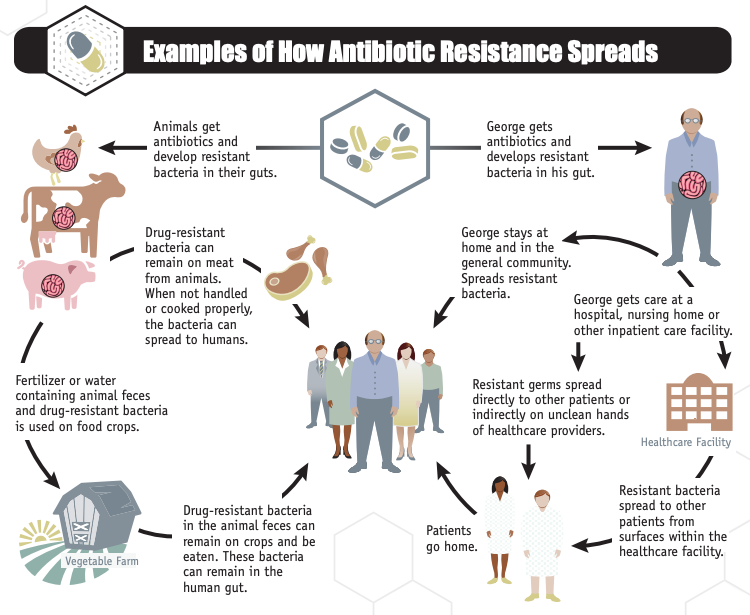
Antimicrobial Resistance (AMR) is the ability of microorganisms such as bacteria, viruses, fungi, and parasites to resist the effects of drugs that once killed them or stopped their growth. It occurs due to the overuse and misuse of antibiotics in humans, animals, and agriculture. AMR makes infections harder to treat, leading to prolonged illness, higher medical costs, and increased mortality. It is a growing global health threat, especially in countries like India with high antibiotic usage and poor regulatory control. The World Health Organisation (WHO) identifies AMR as one of the top 10 global public health threats. Tackling AMR requires a multi-sectoral, One Health approach involving healthcare, veterinary, and environmental sectors.
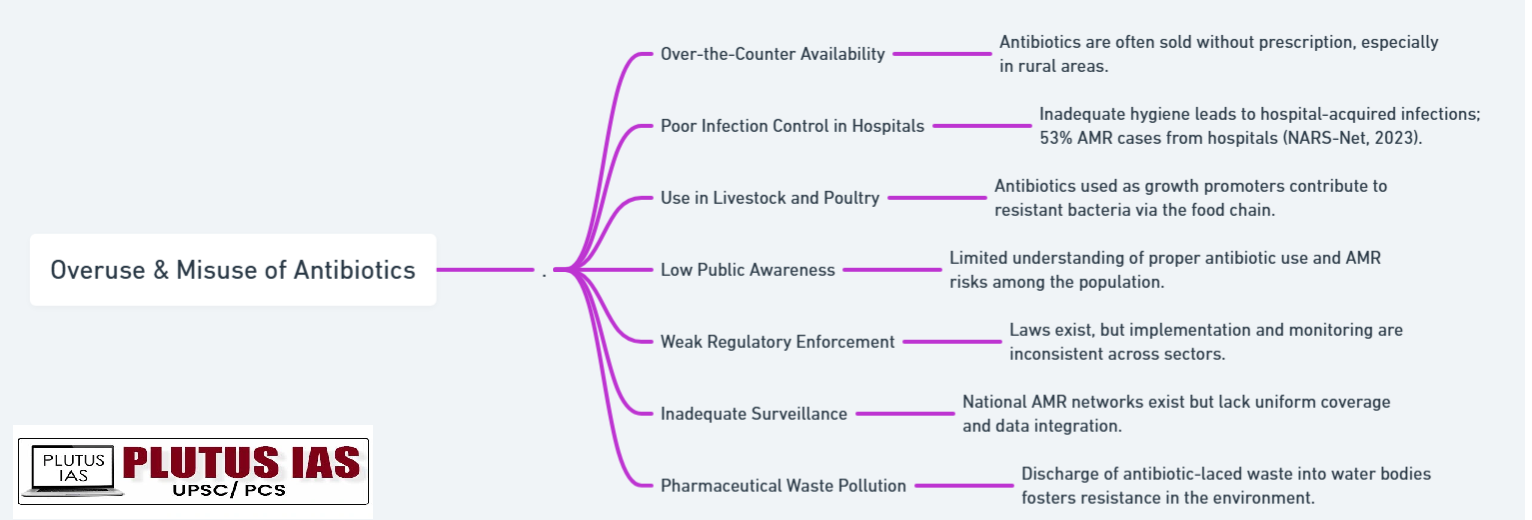
Key Factors Contributing to AMR in India
Recent Developments in AMR
1. Development of Nafithromycin (Nafasyn): India’s Wockhardt developed a new antibiotic (first in over 30 years), effective against respiratory tract infections, requiring just 3 doses.
2. Rise of Indian Antibiotic Innovators: Indian companies like Wockhardt, Bugworks, and GangaGen are advancing antibiotic R&D, contributing to global AMR solutions.
3. Strengthening of National Surveillance (NARS-Net): Expanded surveillance of AMR in hospitals and labs under the National Programme on AMR Containment.
4. Ban on Colistin for Growth Promotion: India banned colistin, a critical antibiotic, in livestock to curb resistance transmission.
5. Promotion of One Health Approach: The Government is integrating human, animal, and environmental health sectors in AMR response policies.
6. Public Health Campaigns: Awareness programs launched by ICMR and MoHFW on rational antibiotic use and infection prevention.
7. Global Recognition of India’s Role: WHO and international platforms acknowledge India’s leadership in tackling AMR through innovation and regulation.
Government Initiatives to Combat Antimicrobial Resistance (AMR)
1. National Action Plan on AMR: Launched to promote awareness, surveillance, infection control, and rational antibiotic use in humans and animals.
2. National Programme on AMR Containment: Strengthens lab capacity, surveillance (NARS-Net), and infection prevention in hospitals.
3. Ban on Colistin in Livestock: Prohibits the use of critical antibiotics as growth promoters to prevent resistance spread.
4. One Health Approach: Integrates human, animal, and environmental health sectors for coordinated AMR response.
5. Antibiotic Stewardship: Encourages rational prescribing and reduces over-the-counter antibiotic sales.
6. Public Awareness Campaigns: Conducted by ICMR and MoHFW to educate on antibiotic misuse and infection prevention.
7. Support for R&D: Promotes the development of new antibiotics and alternative treatments by Indian innovators.
8. International Cooperation: Collaborates with WHO and global partners to tackle AMR worldwide.
Challenges in AMR Management
1. Overuse and Misuse of Antibiotics: Widespread irrational prescribing and self-medication increase resistance.
2. Poor Regulation and Enforcement: Weak control over antibiotic sales and use in humans and animals.
3. Limited Awareness: Lack of public and healthcare worker knowledge about AMR and proper antibiotic use.
4. Inadequate Surveillance: Insufficient data collection and monitoring of resistance patterns, especially in rural areas.
5. Infection Prevention Gaps: Poor sanitation and hygiene in healthcare settings facilitate spread of resistant infections.
6. Environmental Contamination: Antibiotics entering water bodies from pharmaceutical waste and agriculture.
7. Slow Development of New Drugs: Limited investment and innovation in new antibiotics and alternatives.
8. Multi-sectoral Coordination: Difficulty in integrating human, animal, and environmental health efforts effectively.
Way Forward to Combat AMR
1. Strengthen Antibiotic Stewardship: Promote rational use of antibiotics among doctors, pharmacists, and the public.
2. Enhance Surveillance: Expand and improve monitoring of AMR in hospitals, communities, animals, and the environment.
3. Improve Infection Control: Upgrade sanitation, hygiene, and infection prevention measures in healthcare settings.
4. Enforce Regulations: Tighten laws on antibiotic sales and use in humans and livestock.
5. Promote Research and Innovation: Support development of new antibiotics, diagnostics, and alternative treatments.
6. Adopt One Health Approach: Foster collaboration across human, animal, and environmental health sectors.
7. Increase Public Awareness: Conduct sustained education campaigns on AMR and responsible antibiotic use.
8. Strengthen International Cooperation: Share data, best practices, and resources globally to address AMR collectively.
Conclusion
Antimicrobial Resistance (AMR) poses a severe and growing threat to global health, with millions of lives lost each year due to drug-resistant infections. India, with its high antibiotic use and regulatory challenges, faces a critical battle against AMR. The tragic case of Viswanatham highlights the urgent need for coordinated action to prevent misuse of antibiotics, strengthen surveillance, and improve infection control. Through government initiatives, innovation, public awareness, and a One Health approach, India can lead the fight against AMR. Sustained efforts and global cooperation are essential to safeguard the effectiveness of antibiotics and protect future generations from the devastating impacts of resistant infections.
Download Plutus IAS Current Affairs (Eng) 23rd May 2025
Prelims Questions
Q. With reference to the National Action Plan on AMR (India), consider the following statements:
1. It aims to improve surveillance and infection control in hospitals.
2. It encourages unrestricted use of antibiotics in animals to boost productivity.
3. It promotes public awareness campaigns on rational antibiotic use.
How many of the above-given statements are correct?
(a) Only one
(b) Only two
(c) All three
(d) None
Answer: A
Mains Questions
Q. Discuss the challenges posed by Antimicrobial Resistance (AMR) in India. What steps has the government taken to tackle this issue? Suggest ways forward to effectively combat AMR in the country.
(250 words, 15 marks)



No Comments